Diabetes, Prediabetes and Insulin Resistance Services
Address Insulin Resistance with a Personalized Plan
Living with insulin resistance, diabetes, or prediabetes can feel overwhelming. Constant concerns about blood sugar levels, energy fluctuations, and diet adjustments can leave you searching for clarity and control.
With evidence-based tools and individualized support, we empower you with strategies that can help you to lower your A1C levels, improve your overall health and wellness, and increase your energy for the long term.
Transform your health naturally. Schedule your first appointment today.
Why Managing Insulin Resistance Matters
Without taking action, insulin resistance can lead to severe health outcomes, including cardiovascular diseases, neuropathy, and obesity. However, early intervention and a clear treatment plan can reduce the risk of these complications. Research shows that even minor lifestyle adjustments, such as prioritizing whole foods and reducing refined processed foods, staying active through regular exercise, and incorporating healthy fats and lean proteins into meals, can slow and sometimes even reverse the progression to diabetes.
Did You Know?
According to the Centers for Disease Control and Prevention (CDC), 1 in 3 U.S. adults has prediabetes, most without knowing it.
Making sustainable changes early can lower your risk of developing Type 2 diabetes and reduce reliance on medications.
Addressing insulin resistance may lower A1C levels, improve energy, reduce cravings, and support long-term healthy weight maintenance.
Whole Health Partners is here to guide you every step of the way, ensuring you have a clear plan and ongoing support throughout your journey.

Whole Health Partners’ Approach to Diabetes Management
If caught early, it’s often possible to address insulin resistance and prediabetes through lifestyle medicine interventions that include diet, physical activity, sleep hygiene, and stress management. These same strategies can also be applied to more severe cases of insulin resistance, like Type 2 diabetes. While medication is typically necessary in more advanced cases, diet and lifestyle changes can increase the chances of success.
At Whole Health Partners, our personalized, all-encompassing care plan includes:
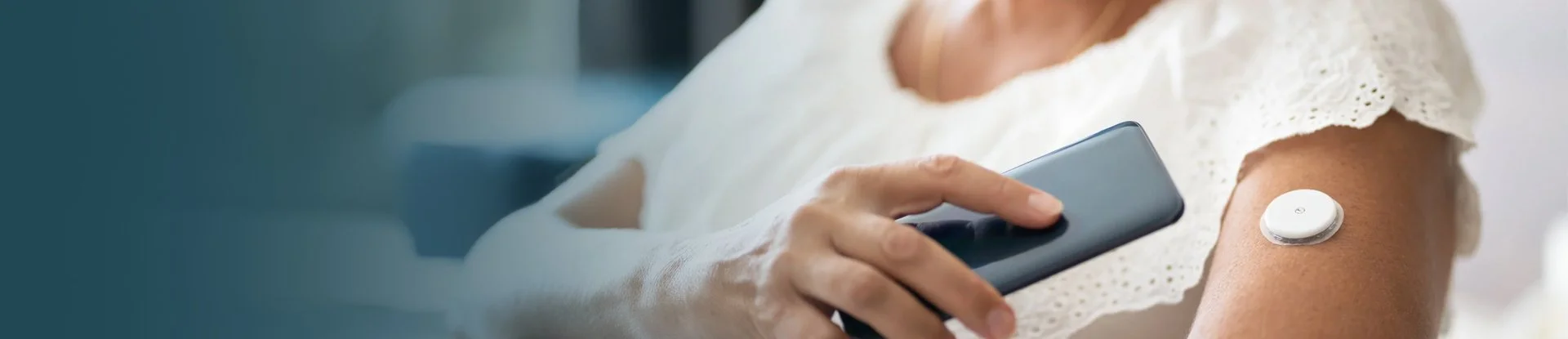
1. Precise Glucose Monitoring
Gain real-time insights into your average blood glucose levels with advanced tools, such as Continuous Glucose Monitoring (CGMs).
2. Customized Nutrition Guidance
Learn which whole foods, portion sizes, and meal strategies work best for your body. (Hint: it’s not about deprivation!)
3. Movement That Empowers
Develop a realistic, joyful exercise plan that fits your life and goals.
4. Sleep Optimization
Find better rest and rejuvenation through tailored sleep hygiene strategies.
5. Stress Management
Gain practical tools to lower cortisol levels and rebalance your body.
We won't give you a generic checklist.
We'll work with you to develop a plan that's specifically designed for you. Our team of doctors and dietitians provides ongoing education, practical strategies, and personalized solutions that fit into your real life for lasting success.
Kind Words
“I went from 178 lbs down to 158 lbs. I was able to lower my A1C, rather quickly, into the normal range and I actually feel like I have some control over my health for the first time in a long while and that feels pretty good”
- Margaret, Whole Health Partners Patient
“I think if you're on the fence of should I do this or should I not, I would say just do it. They're going to meet you where you are and they're going to give you ideas that feel practical in your season of life. [Whole Health Partners] has changed my life.”
- Shyana, Whole Health Partners Patient
Results We'll Help You Aim For
Science-based strategies tailored to you will greatly increase your chances of real, measurable progress. With Whole Health Partners, we'll help you work toward health improvements, including:
Lowered A1C levels
Reduced blood sugar spikes
Improved mood and energy
Empowered food choices and reduced cravings
Long-term weight management tailored to your body
You don’t need to face diabetes or insulin resistance alone. Take the first step toward better health and a brighter future with help from our team of providers.
Frequently Asked Questions
What Is Insulin Resistance?
Insulin resistance occurs when your body doesn’t effectively use insulin to regulate average blood glucose levels, leading to rising blood sugars that may result in conditions like prediabetes and Type 2 Diabetes. Other related issues, such as polycystic ovarian syndrome (PCOS), can also affect insulin sensitivity. Understanding the root cause of this condition is key to effectively managing it.
What Are the Health Risks of Insulin Resistance?
Our bodies require blood glucose, also known as blood sugar, to produce energy for the brain, muscles, and other organs. We derive glucose from foods we consume, especially carbs, but when blood sugar gets too high or too low, side effects can develop. Long-term high blood sugar (hyperglycemia) may damage organs and lead to long-term health conditions like cardiovascular disease, nerve damage, an increased risk of cancer, and kidney disease.
Insulin plays a critical role in regulating blood sugar. When glucose levels increase after eating, the pancreas releases insulin, which allows glucose to enter your muscles and other cells for energy. However, if your body becomes insensitive to insulin due to a combination of genetic, lifestyle, and environmental factors, blood glucose levels can rise to unhealthy levels. Over time, this increases the risk of diabetes, cardiovascular complications, and persistent fatigue.
Common health risks of insulin resistance include:
High blood sugar (over 140 mg/dl)
Increased risk of obesity and weight loss resistance
Long-term reliance on diabetes medications
Metabolic health issues, non-alcoholic fatty liver, Alzheimer’s, and elevated cholesterol levels
What Risk Factors May Lead to Increased Insulin Resistance?
Genetic and lifestyle factors that contribute to insulin resistance include:
Being overweight or obese, especially if carrying excess weight around the belly or organs
Being over 45
Having a close relative—parent or sibling—with diabetes
Physical inactivity
Health conditions like high blood pressure, abnormal cholesterol levels, a history of heart disease, or stroke
It’s important to note that people of specific ethnic backgrounds—including African American, Hispanic/Latino, and Native American—are potentially at higher risk of insulin resistance.
How Can I Tell If I Have Diabetes or Prediabetes?
While insulin resistance can eventually lead to severe health conditions, there are often very few symptoms related to the early stages of pre-diabetes. That’s why it’s essential to have labs taken regularly and, where appropriate, to utilize technology like CGMs to assess how your body processes blood glucose.
The A1C test, also known as the hemoglobin A1C or HbA1C test, is a blood test that measures your average blood sugar levels over the past 2–3 months. It provides a percentage that reflects how much glucose is attached to your red blood cells, giving your healthcare provider insights into your long-term blood sugar management.
An A1C level below 5.7% is considered a healthy range, while levels between 5.7% and 6.4% indicate prediabetes. A result of 6.5% or higher typically signals diabetes.
What Is the A1C Test?
What Reduces A1C Quickly?
Reducing A1C requires a combination of consistent lifestyle changes, including adopting a balanced diet rich in whole, nutrient-dense foods, staying physically active, managing stress, and getting adequate sleep.
Foods high in fiber, such as leafy vegetables, legumes, and whole grains, can help stabilize blood sugar levels. Go easy on carbohydrate-rich foods and starchy vegetables, as these increase your blood sugar levels.
Regular physical activity, such as walking or strength training, improves insulin sensitivity. While rapid changes can occur, sustainable reductions often result from gradual adjustments tailored to your unique needs.
How Long Does It Take to Lower A1C?
Lowering your A1C isn’t an overnight process, as it reflects blood sugar levels over several months. With healthy lifestyle adjustments, noticeable changes may start appearing in as little as three months. However, the time frame varies from person to person, based on factors such as starting A1C level, adherence to changes, and overall health. The key is consistency and patience to create lasting improvement.
Can You Reverse Type 2 Diabetes?
Yes, it’s possible to reverse Type 2 diabetes for some individuals through comprehensive lifestyle changes. Reversal means achieving and sustaining normal blood sugar levels without the need for ongoing medication. This often involves significant changes to diet, exercise, and weight management. However, outcomes differ based on individual health circumstances, and it’s important to work closely with your healthcare provider to create a personalized plan.
Empower Your Health, Your Way
Our clinic serves all North Carolina residents, including the Research Triangle (Raleigh, Durham, and Chapel Hill) and Charlotte, NC. Schedule an appointment today and take the first step toward preventing or reversing diabetes with Whole Health Partners.
Weight Loss
Women’s Health: Hormonal Health, Polycystic Ovarian Syndrome (PCOS), and Perimenopause/Menopause
Diabetes, Pre-Diabetes, Insulin Resistance, and Blood Glucose Management
High Blood Pressure/Hypertension Management
High Cholesterol Management
Lifestyle Medicine